Treatment of Tuberculosis Disease: A Comprehensive Guide
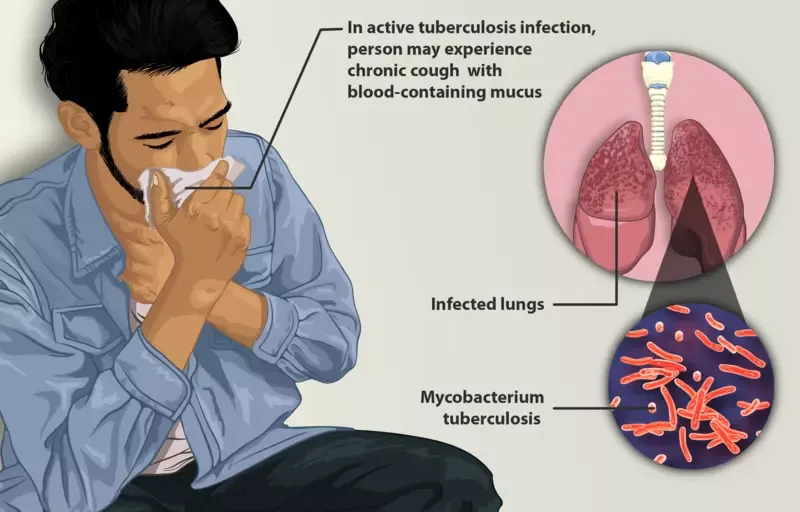
Depiction of a tuberculosis patient, CC BY-SA 4.0, via Wikimedia Commons
Drug-resistant tuberculosis (DR-TB) poses a significant public health challenge, impacting patients, communities, and healthcare systems. This article explores the causes, symptoms, diagnosis, and treatment of tuberculosis, along with preventive measures and side effect management strategies. Discover everything you need to know about tuberculosis treatment, including medications, therapy duration, side effects, and preventive measures.
Our in-depth guide will help you understand the ins and outs of managing and treating TB effectively.
- Understanding Tuberculosis
- Causes and Symptoms of Tuberculosis
- Diagnosis of Tuberculosis
- Standard Treatment Regimen of Tuberculosis
- First-Line Drugs for Tuberculosis Treatment
- Second-Line Drugs and Drug-Resistant TB
- Duration of Treatment
- Who 2022 Recommendations for Drug-Resistant TB Treatment
- Drug-Resistant TB Definitions
- Managing Side Effects
- Preventive Measures
- Frequently Asked Questions (FAQs)
- Final Thoughts
Understanding Tuberculosis 🦠
Tuberculosis (TB) is a potentially severe infectious disease primarily affecting the lungs (↗). Caused by the bacterium Mycobacterium tuberculosis, it can also impact other parts of the body. TB is transmitted through the air when an infected person coughs, sneezes, or talks. Timely diagnosis and appropriate treatment are crucial for preventing the spread of TB and reducing the risk of complications.
Key Facts
- 🦠 In 2021, TB claimed 1.6 million lives, ranking as the 13th top cause of death and the second highest infectious killer after COVID-19
- 🌍 Around 10.6 million individuals contracted TB across the globe in 2021, impacting all nations and age demographics
- 💊 The ongoing public health crisis and security risk is posed by multidrug-resistant TB (MDR-TB)
- 🚑 From 2000 to 2021, TB diagnosis and treatment saved approximately 74 million lives
- 💰 To reach global objectives, US$ 13 billion per year is required for TB prevention, diagnosis, treatment, and care
- 🎯 One of the United Nations Sustainable Development Goals (SDGs) is to eradicate the TB epidemic by 2030 as part of its health targets
Causes and Symptoms of Tuberculosis

Image via Wikipedia
TB is caused by the Mycobacterium tuberculosis bacterium. It primarily spreads through tiny droplets released into the air by infected individuals. People with weakened immune systems (↗) are more susceptible to TB infection.
Common symptoms of TB include:
- Persistent cough lasting more than three weeks
- Coughing up blood or sputum
- Chest pain or discomfort
- Unintentional weight loss
- Night sweats
- Fever
- Fatigue
Diagnosis of Tuberculosis 🔬
Diagnosing TB involves a combination of medical history, physical examination, skin tests, blood tests, and imaging tests like chest X-rays. Early diagnosis is critical for prompt treatment and preventing the spread of the disease.
Standard Treatment Regimen of Tuberculosis
TB treatment usually has two goals: curing the infected person and reducing the spread of the bacteria to healthy people. A combination therapy is often prescribed to completely cure a TB patient, with the exception of latent TB.
First-Line Drugs for Tuberculosis Treatment 💊
The World Health Organization (WHO) provides guidelines for treating drug-susceptible and drug-resistant TB [1]. The WHO recommends a combination of first-line drugs for treating TB. These include:
- Isoniazid (INH or H): A powerful antibiotic that's effective against TB bacteria.
- Rifampin (RMP or R): Kills TB bacteria by targeting their RNA synthesis.
- Ethambutol (EMB or E): Works by inhibiting the bacteria's cell wall synthesis.
- Pyrazinamide (PZA or Z): Effective against dormant TB bacteria in acidic environments.
Each of these drugs plays a vital role in fighting the infection, and they're often used in combination to ensure treatment efficacy. But what if the bacteria become resistant to these drugs?
Second-Line Drugs and Drug-Resistant TB 💉
In cases of drug-resistant TB, such as multidrug-resistant tuberculosis (MDR-TB) or extensively drug-resistant tuberculosis (XDR-TB), second-line drugs are used [2]. The WHO recommends longer treatment regimens for these patients using second-line drugs, depending on the type and extent of drug resistance. These include:
- Fluoroquinolones: e.g., Levofloxacin and Moxifloxacin.
- Injectable agents: e.g., Amikacin, Kanamycin, and Capreomycin.
- Other oral agents: e.g., Cycloserine, Linezolid, and Para-Aminosalicylic Acid (PAS or P).
These drugs are reserved for special situations and are often used alongside first-line drugs to increase treatment effectiveness.
Thioacetazone was previously listed as a first-line drug for TB treatment. However, the WHO's revision to the "Treatment of Tuberculosis" recommendations (4th edition) no longer lists this drug as one of the first-line treatments.
Duration of Treatment ⏳
The standard treatment regimen for TB involves daily doses of Isoniazid and Rifampin for six months. Ethambutol and Pyrazinamide are administered daily for the initial two months. This regimen can be used for both pulmonary and extrapulmonary TB. However, a 12-month course may be necessary for certain extrapulmonary TB cases.
Who 2022 Recommendations for Drug-Resistant TB Treatment
| # | Recommendation | Details | Evidence |
|---|---|---|---|
| 1 | 6-month BPaLM regimen for MDR/RR-TB and pre-XDR-TB | Bedaquiline, pretomanid, linezolid (600 mg), and moxifloxacin for MDR/RR-TB patients | Conditional, very low certainty |
| 2 | 9-month all-oral regimen for MDR/RR-TB | For patients without fluoroquinolone resistance | Conditional, very low certainty |
| 3 | Longer regimens for MDR/RR-TB | Includes various recommendations for specific agents and durations | Conditional, very low to moderate certainty |
| 4 | Regimen for rifampicin-susceptible, isoniazid-resistant TB | 6-month treatment with rifampicin, ethambutol, pyrazinamide, and levofloxacin | Conditional, very low certainty |
| 5 | Monitoring patient response to MDR/RR-TB treatment using culture | Perform sputum culture alongside sputum smear microscopy | Strong, moderate certainty |
| 6 | Starting antiretroviral therapy in patients on MDR/RR-TB regimens | Initiate ART for all HIV-positive patients within the first 8 weeks of anti-TB treatment | Strong, very low certainty |
| 7 | Surgery for patients on MDR/RR-TB treatment | Elective partial lung resection (lobectomy or wedge resection) alongside a recommended MDR-TB regimen | Conditional, very low certainty |
Drug-Resistant TB Definitions
| # | Term | Definition |
|---|---|---|
| 1 | Drug-resistant TB (DR-TB) | A form of TB caused by Mycobacterium tuberculosis complex strains that are unresponsive to any TB medications |
| 2 | Extensively drug-resistant TB (XDR-TB) | A TB variant caused by M. tuberculosis complex strains resistant to rifampicin (possibly isoniazid as well), one fluoroquinolone (levofloxacin or moxifloxacin), and one "Group A" drug (bedaquiline or linezolid) |
| 3 | MDR/RR-TB | Encompasses both multidrug-resistant TB (MDR-TB) and rifampicin-resistant TB (RR-TB) |
| 4 | Multidrug-resistant TB (MDR-TB) | TB caused by M. tuberculosis complex strains that show resistance to both rifampicin and isoniazid |
| 5 | Pre-extensively drug-resistant TB (pre-XDR-TB) | TB caused by M. tuberculosis complex strains resistant to rifampicin (possibly isoniazid as well) and at least one fluoroquinolone (levofloxacin or moxifloxacin) |
| 6 | Rifampicin-resistant TB (RR-TB) | TB caused by M. tuberculosis complex strains that are resistant to rifampicin, with varying susceptibility to isoniazid and other first-line or second-line TB medicines |
| 7 | Rifampicin-susceptible, isoniazid-resistant TB (Hr-TB) | TB caused by M. tuberculosis complex strains that are resistant to isoniazid but remain susceptible to rifampicin |
Managing Side Effects 🚑
While TB medications are effective, they can also cause side effects. It's essential to monitor and report any side effects to your healthcare provider. Some common side effects include:
- Nausea and vomiting (↗)
- Loss of appetite
- Jaundice (yellowing of the skin and eyes)
- Dark urine
- Fatigue or weakness
- Tingling or numbness in hands and feet
- Visual disturbances
Your healthcare provider can recommend ways to manage these side effects, adjust your medication, or switch to alternative drugs if needed.
Preventive Measures 🛡️
In addition to treatment, it's crucial to take preventive measures to reduce the risk of TB infection and transmission. Some steps include:
- Vaccination: The Bacillus Calmette-Guérin (BCG) vaccine is available for infants and high-risk individuals in some countries.
- Proper ventilation: Ensure good airflow in living spaces to reduce the concentration of TB bacteria in the air.
- Face masks: Use masks when in close contact with TB patients or in crowded, poorly ventilated spaces.
- Follow-up care: Regular check-ups and monitoring during and after treatment are essential for preventing relapse and drug resistance.
By following these preventive measures and adhering to the prescribed treatment regimen, you can effectively manage TB and prevent its spread.
Frequently Asked Questions (FAQs)
What is the main cause of tuberculosis?
Tuberculosis is primarily caused by the bacterium Mycobacterium tuberculosis, which spreads through the air when an infected person coughs, sneezes, or talks.
What are the 3 types of tuberculosis?
The three types of tuberculosis are: latent TB (inactive and non-contagious), active TB (symptomatic and contagious), and drug-resistant TB (resistant to standard medications).
Is tuberculosis curable now?
Yes, tuberculosis is curable with proper medical treatment, including a combination of antibiotics taken over several months.
Is TB life threatening?
TB can be life-threatening if not properly treated, especially in cases of drug-resistant TB or in individuals with weakened immune systems.
How long do TB patients live?
With appropriate treatment, TB patients can fully recover and live normal, healthy lives. However, if left untreated, TB can be fatal.
Can TB cause death?
Yes, untreated or improperly managed TB can lead to death, making it essential to seek medical care and follow the prescribed treatment regimen.
Who is most at risk for tuberculosis?
Those at higher risk for tuberculosis include people with weakened immune systems (e.g., HIV/AIDS patients), those in close contact with infected individuals, and individuals living or working in crowded settings (e.g., prisons, shelters).
How long can TB cause death?
The time it takes for TB to cause death varies depending on factors such as the severity of the disease, the patient's overall health, and whether treatment is initiated promptly. However, without treatment, TB can be fatal within months to years.
Can you live a long life with TB?
Yes, if TB is diagnosed and treated effectively, patients can fully recover and live long, healthy lives. Early detection and adherence to the prescribed treatment plan are crucial for a successful outcome.
Final Thoughts 🎁
In summary, the treatment of tuberculosis involves a combination of first-line drugs, with second-line drugs reserved for drug-resistant cases. The standard treatment duration is six months, but this may be extended in specific cases. Managing side effects and taking preventive measures are crucial aspects of TB treatment. Remember, early diagnosis and proper medical care can save lives and reduce the risk of transmission. Stay informed and consult your healthcare provider for personalized advice.
Medical References
- World Health Organization. WHO consolidated guidelines on tuberculosis. Module 4: treatment-drug-resistant tuberculosis treatment, 2022 update. World Health Organization; 2022 Nov 30.
- Kuaban C, Noeske J, Rieder HL, Aït-Khaled N, Abena Foe JL, Trébucq A. High effectiveness of a 12-month regimen for MDR-TB patients in Cameroon. The International Journal of Tuberculosis and Lung Disease. 2015 May 1;19(5):517-24.
Recommended Reading
- Understanding Zollinger-Ellison Syndrome: Symptoms, Diagnosis, and Treatment (↗️)
- Irritable Bowel Syndrome: Causes, Symptoms and Treatment (↗️)
- Symptoms and Treatments of Tonsil Stones and Bad Breath (↗️)
- How to Recognize, Prevent, and Treat the Pain that is Carpal Tunnel (↗️)
- Disease of Male Reproductive System: Erectile Dysfunction Explained (↗️)


