Climbing the WHO Pain Ladder: Understanding Pain Medications
Dealing with chronic pain is tricky for both doctors and patients. There are many painkillers available, making it hard to pick the right one. Opioids are often a first-choice group of medications for treating patients with chronic pain, but most doctors avoid prescribing them due to their potential side effects such as physical dependence.
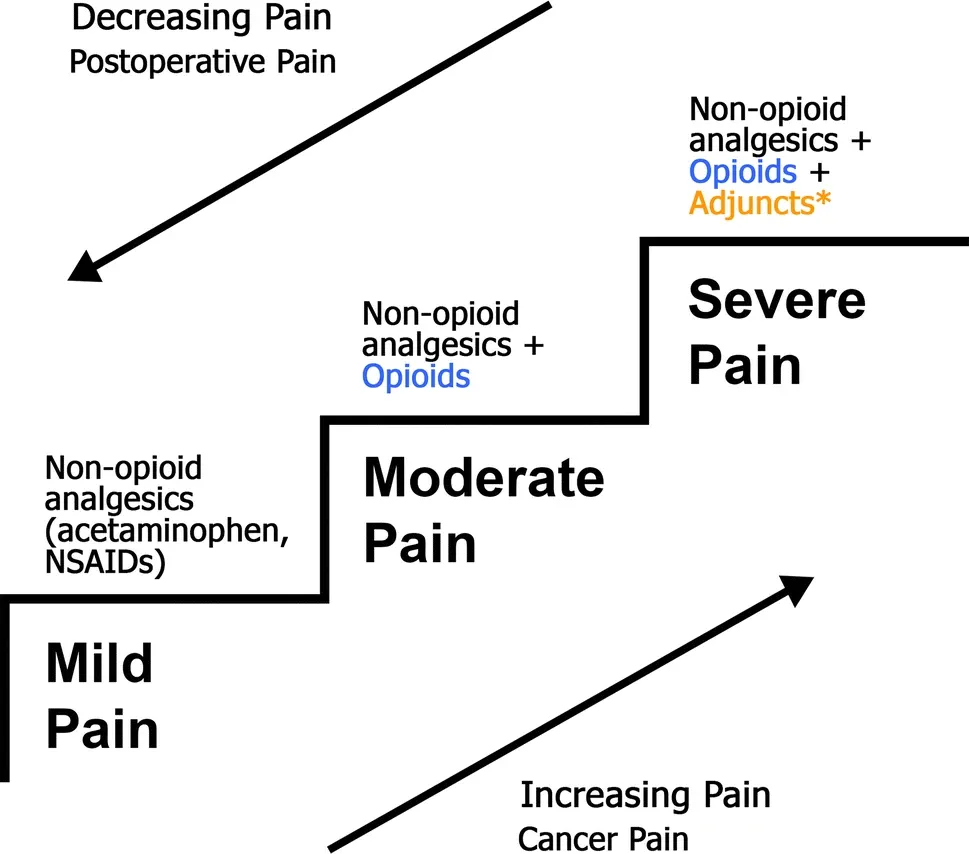
To address this problem, the World Health Organization (WHO) developed the pain ladder. This approach starts with less strong painkillers and gradually increases to the most potent opioids if needed. This way, doctors and patients work together to find the best mix of medicines that control pain with the smallest amount of opioids.
Non-Opioid Analgesics
Non-opioid analgesics are generally the medications found over the counter. For instance, the non-steroidal anti-inflammatory drugs (NSAIDs), such as Advil and Aleve, should be used first when attempting to address a patient’s pain. Prescription strength alternatives to these over the counter NSAIDs, such as high dose ibuprofen, are also an important first step in the pain ladder. Some patients have great pain relief with these medications, but some experience no effect.
Strong NSAIDs are also available by prescription, such as Celebrex and Voltaren, and are also part of this rung of the ladder. They can sometimes treat pain when others do not. Aspirin and acetaminophen should not be ignored, either, as they can help some patients with mild pain.
Recommended Reading: Five Practical Tips to Cope with Back Pain.
Adjuvant Analgesics
Adjuvant analgesics are the newest members of the pain ladder family. These are medications that are traditionally used for other conditions, specifically depression and seizures. Although the usage of these medications for pain is a new concept, researchers have been testing their efficacy as analgesics for a long time. For instance, the tricyclic antidepressants, such as amitriptyline, have been used for decades in treating chronic pain.
Newer depression medications are also used for pain relief. In fact, Cymbalta is the first drug approved by the FDA for the treatment of chronic pain. Anti-seizure medications are helpful, particularly for nerve related pain. Gabapentin’s ability to treat peripheral neuropathy has been well documented, but recent drugs in this category, such as Lyrica, are more effective. When these drugs are combined with a non-opioid analgesic, it can often control the manifestation of chronic pain.
Weak Opioids
Weak opioids are medications that have a small amount of narcotic medication in them, but they are usually combined pharmacologically with a non-opioid analgesic. Medications in this subset include codeine, Darvocet, dihydrocodeine, and Tramadol. These medications are generally prescribed for mild pain, but when they are combined with the non-opioid and adjuvant analgesics, they often completely relieve pain.
The weaker opioids have less risk of side effects, such as nausea, constipation, and sedation. They also have less risk of dependency, and this makes them attractive as treatment for chronic conditions. It is the combined effect of this medication with the previous two categories that forms a cocktail that is quite effective against moderate to severe pain.
Strong Opioids
Strong opioids are used when the previous medications fail to control pain. These medications include morphine, hydrocodone, oxycodone, and fentanyl, among many others. When prescribing these medications, the weaker opioid is replaced with the stronger one, and the non-opioid and adjuvant remain in place. This allows for the prescriber to use the least amount of the strong opioid as possible.
However, the use of strong opioids has some side effects. Many patients report feeling nausea, and the sedation is often severe. In addition, constipation is an important concern, because high dose opioids can slow down the gastrointestinal motility. This usually is addressed with stool softeners and laxatives. The possibility of dependency is greater with these medications, although it is less likely when they are taken as prescribed.
Recommended Reading: Irritable Bowel Syndrome: Causes, Symptoms and Treatment.
Climbing the Ladder
The pain ladder helps doctors treat pain with the least strong drugs first. Patients usually start with non-opioid painkillers, some even available over the counter. If these aren't enough, doctors may prescribe stronger NSAIDs.
If non-opioids don't help, doctors might add another type of medicine called an adjuvant, which is often used for nerve pain. However, these can have serious side effects, so they must be used carefully.
If there's still pain, a weak opiate might be introduced. Some experts are skeptical about this step because these opiates might not be effective and could have risks. But they're considered because they're less likely to lead to addiction.
The last resort is strong opiates, started at low doses and increased until the pain is manageable or side effects become too much. These are usually used with the other medicines to tackle the pain from all sides.
Reference
- Gai N, Naser B, Hanley J, Peliowski A, Hayes J, Aoyama K. A practical guide to acute pain management in children. Journal of anesthesia. 2020 Jun;34:421-33.


